
The diagnosis of "cervical osteochondrosis" is often made if a person complains of neck pain. Some also attribute dizziness, memory loss, numbness of the hands and other unpleasant symptoms to it. It is mistakenly believed that the disease is associated with wear and age-related deformation of the intervertebral discs and other elements of the spinal column.
How does the cervical spine work?
The cervical region consists of 7 vertebrae. Between them are intervertebral discs - semi-rigid structures with a dense ring along the periphery and a jelly-like center, which act as shock absorbers. To the right and left of each vertebra there are two joints, between which protrude the surfaces of the vertebral processes, covered with cartilage. The joints are connected by ligaments and muscles of the back.
Why does neck pain occur?
Typically, neck pain occurs in response to awkward movement, injury, or due to inflammation of any of the structures of the cervical spine. In addition, the cause of pain can be overstretching of muscles or ligaments, for example, when lifting weights, unsuccessfully turning the head, or against the background of arthrosis of the very joints between the articular processes. "Nerve entrapment", or cervical radiculopathy, specific processes (metastases, tumors of the vertebrae, spinal cord membranes in the cervical region) are relatively rare.
26% of men and 40% of women over 30 years of age have experienced neck pain in the past month, and 5% of men and 7% of women feel it all the time.
Acute neck pain usually goes away on its own within 1–2 weeks. Chronic pain in most cases appears due to a lack of physical activity or, on the contrary, too intense exercise.
However, people often mistakenly call unexplained pain and discomfort in the neck cervical osteochondrosis and associate its development with wear and age-related deformation of the intervertebral discs and other elements of the spinal column. But such pain, as a rule, has nothing to do with real osteochondrosis.
Cervical osteochondrosis
According to the International Classification of Diseases (ICD), osteochondrosis (osteochondropathy) is a group of rare hereditary diseases associated with disruption of the normal development and growth of bones. As a rule, osteochondrosis begins in childhood and is severe: part of the joint or bone is deformed, and sometimes even dies. With this disease, it is most often not the cervical spine that is affected, but the thoracic spine (lower thoracic vertebrae). Hence the main clinical manifestation of osteochondrosis is a pronounced curvature of the thoracic spine, the so-called thoracic kyphosis.
Symptoms associated with damage to the thoracic spine:
- dyspnea,
- constant weakness
- inability to breathe fully,
- pain and burning behind the sternum,
- attacks of rapid heartbeat.
Conditions accompanied by neck pain
Cervical spondylosis
In people over 50, neck pain is usually caused by cervical spondylosis, age-related wear and tear of the vertebrae and related structures. With this disease, the intervertebral discs become dehydrated and flattened, causing depreciation in the cervical region to worsen, and many movements are accompanied by pain.

But changes in the spine as we age are normal. So, its structures begin to wear out after an average of 30 years, and by the age of 60, 9 out of 10 people already have cervical spondylosis. However, in most people it is asymptomatic.
Other reasons
Less commonly, neck pain occurs due to hypothermia or severe stress, due to herniated discs or abnormalities of the cervical vertebrae - bone growths (spurs) that compress the nerves extending from the spinal cord.
The most common source of pain in the cervical spine and shoulder girdle is excessive tension (defense) of the muscles: trapezius, long back muscles of the cervical spine.
In addition, the muscles of the cervical spine are closely connected to the aponeurosis - a wide tendon plate that envelops the head. The muscular elements of the aponeurosis in the occipital, temporal and frontal regions connect to the muscles of the cervical region, so neck pain is often accompanied by headache. Thus, neck pain, which appears after prolonged sedentary work or sleeping in an uncomfortable position and is combined with a headache, in most cases is associated with a lack of physical activity and incorrect posture and is not dangerous to health.
The phenomenon of tech neck, the so-called techno-neck or neck of the Internet era, is associated with pain arising due to an uncomfortable posture. Techneck is the result of constant use of a computer and smartphone, due to which a person is forced to bend his neck. The fact is that the relative mass of the head increases with forward tilt. Thus, in the "straight" position, the average weight of an adult’s head is 5 kg. If you tilt your head forward at least 15°, the load on the neck muscles will be 13 kg, at 30° - 20 kg, at 60° - 30 kg. As a result of constant overload, the neck muscles are overstrained, microtraumas, inflammation, fibrosis (overgrowth of connective tissue) and, accordingly, pain can occur.
Reasons contributing to the development of degenerative changes in the cervical spine
The occurrence of pain in the cervical spine is facilitated by birth or any other injuries of the spine, anomalies of its development, postural disorders, muscle dystonia, as well as prolonged immobilization, obesity, and some autoimmune diseases.
- Long-term immobilization is a condition in which a person, due to an underlying disease, is forced to lie down for more than a month. As a result, the muscles weaken - and during verticalization, when the load on them increases, they become excessively tense. Pain occurs.
- Obesity: Excess body weight increases stress on the spinal structures and can cause pain.
- Autoimmune diseases in which cartilage tissue is destroyed (autoimmune arthritis, polychondritis) also lead to neck pain.
Stages of degenerative changes in the cervical spine
There are 4 main stages of degeneration (destruction) of the cervical spine:
- Stage I: intervertebral discs become thinner, mild discomfort appears in the neck area;
- Stage II: intervertebral discs are deformed, the distance between the vertebrae is reduced. The pain increases with movements in the cervical spine;
- Stage III: cartilage and vertebrae rub against each other, neck pain becomes constant, and movements become limited. With very severe deformities of the cervical spine, vertebral artery syndrome may occur with visual and vestibular disturbances, headache;
- IV stage: degenerative changes are pronounced, movements in the cervical spine are very limited and painful. The neck area can be almost completely immobilized.
Symptoms of degenerative changes in the cervical spine
Most people with cervical osteochondrosis experience chronic aching pain and neck stiffness. As the disease progresses, other symptoms may appear (especially if the spinal roots, vertebral artery and adjacent nerve plexuses are compressed).
Symptoms of degenerative changes in the cervical spine:
- neck pain that gets worse with movement or standing;
- pain radiates to the shoulder or arm;
- numbness, tingling, and weakness in the arms and hands;
- clicking or grinding in the neck (especially when turning the head);
- headache;
- attacks of dizziness;
- impaired coordination of movements;
- loss of bladder or bowel control.
If such symptoms appear, you should consult a neurologist as soon as possible.
Types of symptoms of "cervical osteochondrosis"
All symptoms of "cervical osteochondrosis" can be conditionally classified into 3 groups, or syndromes: vertebral, radicular and vertebral artery syndrome.
Symptoms of vertebral (spinal) syndrome:
- crunch in the neck when moving;
- limited mobility;
- violation of the location of the vertebrae relative to each other in the neck;
- smoothing of natural cervical lordosis or lateral curvature in the cervical spine (can only be seen on x-ray, MRI or CT).
Symptoms of radicular syndrome:
- numbness of the fingers on one or both hands;
- shooting, burning pain in the neck, radiating to the arm or both arms;
- dystrophy of the muscles of the neck and arms.
Symptoms of vertebral artery syndrome:
- paroxysmal dizziness, up to loss of consciousness;
- sudden jumps in blood pressure;
- noise in ears;
- blurred vision or spots in the eyes;
- loss of balance and attacks of nausea when moving the head;
- headache (severe pain on one side or both sides).
Diagnosis of degenerative changes in the cervical spine
To understand the cause of neck pain and make a diagnosis of "degenerative changes in the cervical spine" (commonly called cervical osteochondrosis), the doctor will need to conduct an examination, study the medical history, evaluate the results of laboratory tests and instrumental examinations.
The diagnosis and treatment of cervical osteochondrosis is carried out by a neurologist.
Inspection
During the examination, the doctor will listen to the patient’s complaints, clarify the details of the medical history and conduct an examination: check reflexes, muscle strength, sensitivity, and the condition of the vestibular apparatus.
With "cervical osteochondrosis, " visible areas of muscle atrophy (muscle loss), decreased or increased muscle tone of the long back muscles, and static disturbances in the cervical region may be observed in the neck area. When palpating the muscles, a person complains of soreness, and when tilting the head, the pain may radiate to the head or arms, and dizziness or headache may occur.
In addition, patients may experience motor disturbances in the hands (weakness), problems with vision and hearing.
The doctor may also ask the patient to walk, stand on one leg with their eyes closed, or touch their nose. This way, the specialist will be able to assess whether coordination of movements is impaired, whether there are problems with gross and fine motor skills.
Laboratory diagnostics
To assess the general condition of the bones, patients with suspected cervical osteochondrosis are prescribed blood tests for total and ionized calcium, as well as markers of bone tissue growth and destruction - osteocalcin and osteoprotegerin, alkaline phosphatase.
With progressive cervical osteochondrosis, the joints are destroyed, the calcium content may be reduced, and osteocalcin and osteoprotegerin, on the contrary, increased.
Total creatine kinase is also considered a marker of muscle tissue destruction in myositis of the cervical muscles.
In addition, the doctor may need to evaluate the blood levels of microelements involved in the regulation of muscle tone: magnesium, potassium, sodium.
Instrumental diagnostics
To establish the cause of neck pain and associated disorders, imaging studies are necessary: radiography of the cervical spine, computed tomography and magnetic resonance imaging, electroneuromyography.
- Radiography.Using X-rays, you can identify bone deformations, malignant tumors, and degenerative changes in the joints.
- Computed and magnetic resonance imagingperformed if pathology of the spinal column, spinal cord or brain is suspected. Computed tomography shows hemangiomas of the vertebral bodies and gross deformities of the cervical spine. Magnetic resonance imaging is more informative for visualizing muscles, roots, and spinal cord.
- Electroneuromyography- a method for studying the efficiency of impulse transmission along a nerve fiber using low-intensity electric current. The test may be slightly uncomfortable. The study helps clarify the conduction of impulses along the roots, nerves and from nerves to muscles, confirm damage to nerves or muscles and clarify the nature and level of damage.
Treatment of degenerative changes in the cervical spine
The main goals of treating degenerative changes in the cervical spine are to relieve pain, prevent compression of the nerves in the neck, and restore cervical mobility.

Depending on the severity of the condition, the doctor may prescribe medications, physical therapy, or massage. Surgery may be required if nerves are pinched or joints become deformed.
Drug treatment of degenerative changes in the cervical spine
Neck pain can be relieved with medication.
Medicines to relieve neck pain and stiffness:
- local anesthetic ointments, gels and patches;
- non-steroidal anti-inflammatory drugs;
- hormonal drugs in the form of tablets or injections into the area of the affected joint;
- muscle relaxants to relieve muscle spasms;
- antidepressants to relieve chronic pain.
Non-drug treatment of cervical osteochondrosis
Along with drug therapy, it is important for patients with cervical osteochondrosis to do neck exercises. For this purpose, the person is referred to a physiotherapist for consultation. It teaches how to properly stretch and strengthen the muscles of the neck and shoulders.
Your doctor may recommend mats or rollers with metal or plastic needles. They are used for 15-30 minutes before bed to relax muscles.
Wearing a Shantz splint (neck brace) is a passive exercise therapy for the deep muscles of the cervical region, which are difficult to influence with exercise. When a person puts on a splint, the muscles relax, and when they take them off, they tense up. If you wear a splint for 15-20 minutes several times a day, you can train and strengthen them.
It only makes sense to wear it for 2–3 hours if you have serious neck injuries. In addition, you should not lie in it, much less sleep.
Surgical treatment of degenerative changes in the cervical spine
As a rule, surgery is required for patients with severe deformation of the spinal column who have a pinched nerve.
During the operation, the surgeon removes pathological elements (hernial protrusions, formations, etc. ) or part of the vertebra. After such treatment, a long period of rehabilitation is required: wearing a Shants splint or a rigid splint for the cervical spine, physiotherapy, regular walking, painkillers.
Complications and consequences of degenerative changes in the cervical spine
Without treatment, the intervertebral discs gradually wear out and the vertebrae are "erased. "
Common complications of degenerative changes in the cervical spine:
- intractable pain syndrome in the head, neck, chest;
- cramps, movement disorders and numbness of the hands;
- frequent dizziness, impaired coordination of movements, fine and gross motor skills.
Prevention of degenerative changes in the cervical spine ("cervical osteochondrosis")
There is no specific prevention of true cervical osteochondrosis, because it is a hereditary disease.
To avoid the appearance of nonspecific neck pain, which is mistakenly associated with cervical osteochondrosis, it is important to ensure correct posture and be physically active: the more a person moves, the better the condition of the muscles, bones, ligaments and joints.
To maintain physical activity, adults need 150 minutes of moderate-intensity aerobic activity per week. Fast walking, swimming, cycling, tennis, dancing or rollerblading are suitable. Pilates and yoga will help strengthen your muscles.
In addition, gymnastics helps to avoid overstraining the neck muscles and the appearance of pain: tilting the head forward, backward, alternately to each shoulder and rotating it, as well as sleeping on an orthopedic pillow.
You should avoid injuries to the cervical spine: do not jump into the water upside down, wear seat belts in the car (prevention of whiplash injury in an accident).

Sleeping position for back pain
Pain in the neck and back, which is often attributed to osteochondrosis, may be the result of an uncomfortable sleeping position.
During sleep, the head and spine should be approximately at the same level. This position minimizes additional pressure on the neck area.
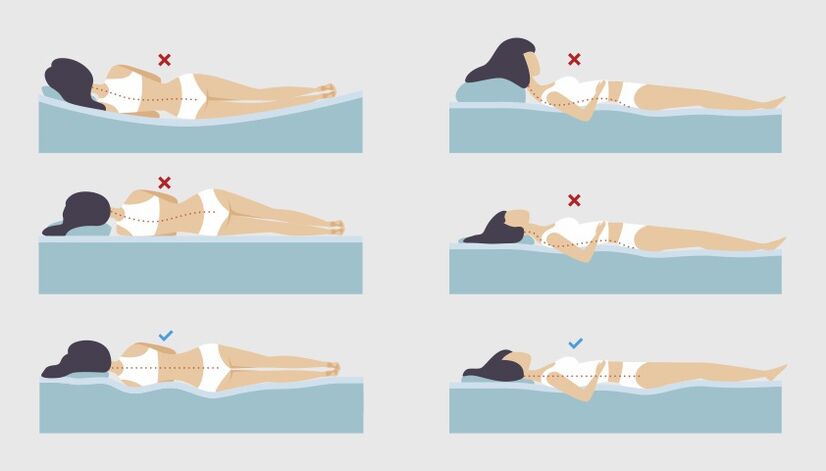
If a person sleeps mainly on his back, the height of the pillow should be on average 6–11 cm. For those who sleep on their side, the pillow should be thicker: from 9 to 13 cm. This way, the desired angle will be maintained between the shoulder and head, the cervical spine will not sag, and the muscles strain to compensate for the inconvenience.
Moreover, the greater the person’s weight, the higher the pillow should be. You also need to pay attention to the hardness of the mattress. The softer it is, the more it will sag under the weight of the body and the higher the pillow should be. In addition, it is better not to always sleep on only one side - this leads to muscle imbalance.
If a person prefers to sleep on his stomach, he may more often suffer from back and neck pain. The fact is that in this position it is difficult to keep the spine in a neutral position. To relieve tension from your back, you can put a pillow under your pelvis and lower abdomen, and choose a flat pillow under your head, or even sleep without one.
In addition, you can use a special orthopedic pillow.
FAQ
- Where can pain radiate from "cervical osteochondrosis"?
Pain from degenerative changes in the cervical spine can radiate to the shoulder or arm, and also intensify with movement or standing.
- How to relieve an attack of dizziness with "cervical osteochondrosis"?
To relieve an attack of dizziness, you should take a comfortable position in which the likelihood of falling is minimal (sit in a chair with back support or lie down) and call for help. After 5–7 minutes, you can try to turn your head: most likely, the attack of dizziness will pass during this time. If dizziness persists or worsens, nausea, vomiting or other neurological symptoms (impaired speech, vision, movement, swallowing, sensitivity) appear, you should call an ambulance as soon as possible.
- How to sleep correctly with "cervical osteochondrosis"?
During sleep, the head and spine should be approximately at the same level. This position minimizes additional pressure on the neck area.
- How long does an exacerbation of "osteochondrosis" of the cervical spine last?
On average, exacerbation of symptoms due to degenerative changes in the cervical spine ("cervical osteochondrosis") lasts from 4 to 7 days. Non-steroidal anti-inflammatory drugs and muscle relaxants are used to reduce pain. During this time, it is better for a person to remain calm and wear a neck brace.
- Which doctor treats "osteochondrosis" of the cervical spine?
Diagnosis and treatment of pain in the cervical region is carried out by a neurologist, neurosurgeon, orthopedist, and general practitioner.















































